What is the CMS 1500 Claim Form
What is the CMS 1500 Claim Form
Blog Article
An essential guide to understanding and using the CMS 1500 Claim Form for insurance billing and reimbursement in healthcare. The CMS 1500 Claim Form is a standardized billing document used by healthcare providers, such as physicians and specialists, to submit claims to insurance companies for services provided to patients. This essential form ensures that providers are reimbursed properly and efficiently for the healthcare services they render. At Mastermind Healthcare, we understand the importance of this form in ensuring a smooth and seamless billing process. Whether you're a healthcare provider looking to streamline your claim submissions or a patient curious about how the process works, this guide will help clarify everything you need to know about the CMS 1500 Claim Form and how it helps providers get reimbursed. The CMS 1500 form is crucial for several reasons: At Mastermind Healthcare, we guide healthcare providers through the process of accurately completing and submitting the CMS 1500 form, ensuring a smooth and timely reimbursement cycle. The process of using the CMS 1500 Claim Form typically involves the following steps:
What is the CMS 1500 Claim Form? A Complete Guide

What is the CMS 1500 Claim Form? A Complete Guide by Mastermind Healthcare
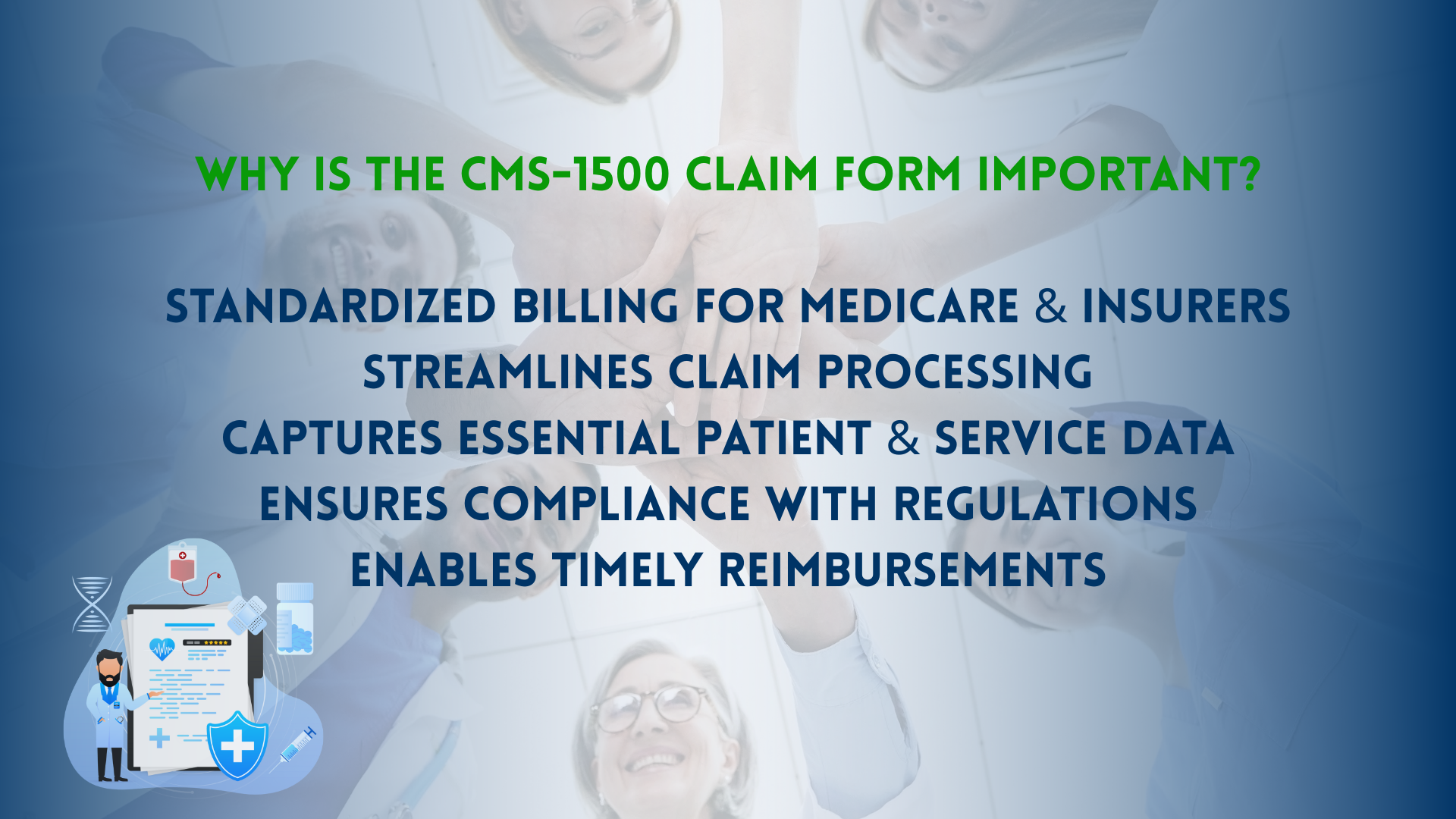
Why is the CMS 1500 Claim Form Important?
How Does the CMS 1500 Claim Form Work?